Bariatric Surgery
Bariatric surgery is designed to help patients address obesity and significantly improve their overall health.
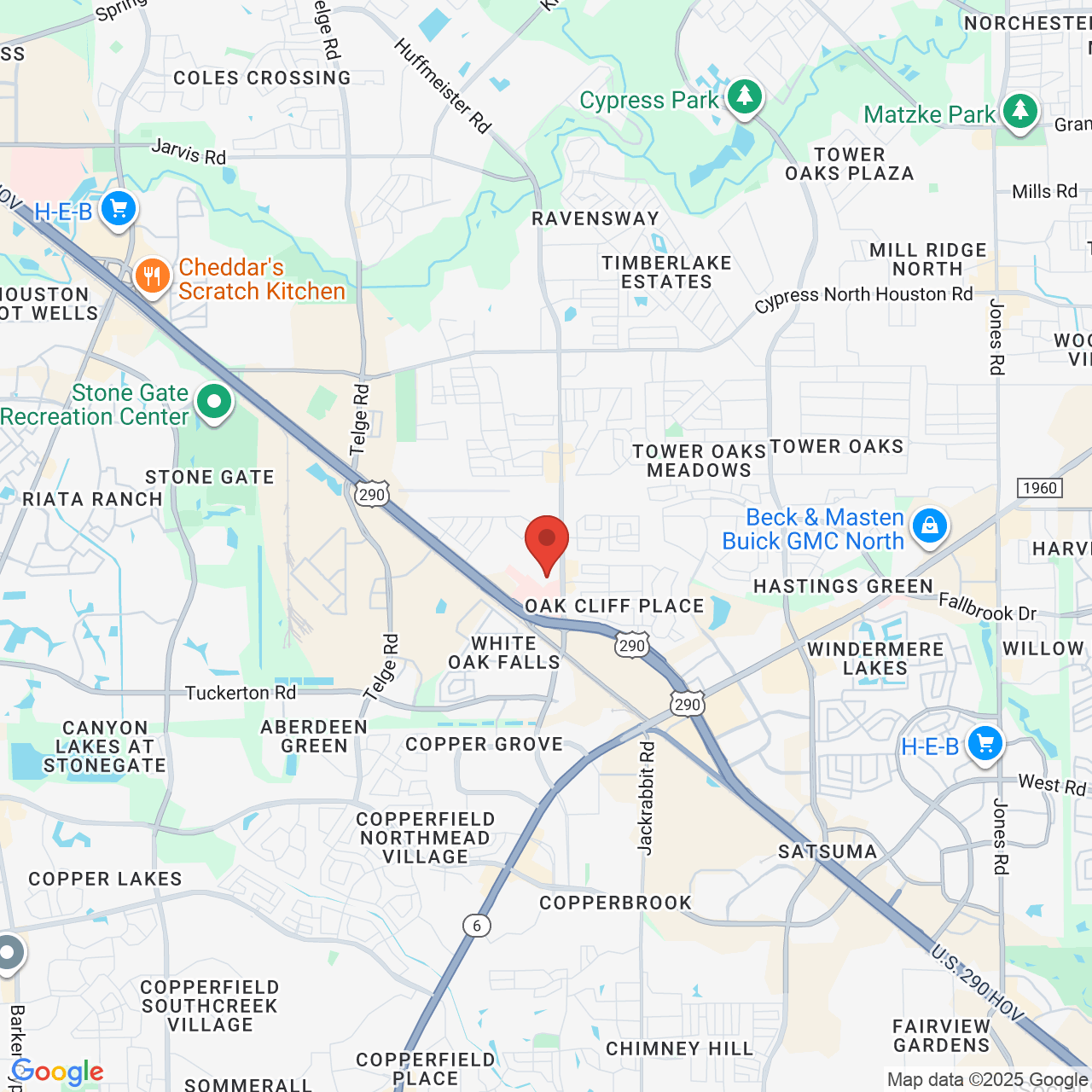
Dr. Matthew St. Laurent of Houston, TX, offers several different types of bariatric surgery in order to meet the diverse needs of patients.
If you are interested in weight loss surgery, schedule a consultation with the team at Northwest Endosurgical today.
John's Story
Interested? Find Out If You Qualify
If you're considering bariatric surgery as an option for weight loss, our surgeon makes it easy to find out if you qualify. Our 60-second survey gives you personalized results and guidance based on questions like your height and weight and if you have any metabolic diseases.
This survey is not intended to replace our Houston bariatric surgeon's opinion but can help you learn if weight loss surgery is right for you.

Get The Process Started
Request a Consultation
If you have been unable to lose weight through diet and exercise, surgical intervention may be what you need to overcome obesity and metabolic diseases. At Northwest Endosurgical, we serve greater Houston from our office in Cypress, TX, and help patients like you experience long-term, healthy, sustainable weight loss through bariatric surgery.
Are you wondering if weight loss surgery is right for you? Contact us today to schedule a personal consultation with Dr. St. Laurent.
Call Us: (281) 921-1890
5-Star Reviews
I visited Dr. St. Laurent to go over issues I have that have developed over time. The office is beautiful and the staff that I worked with were wonderful. Dr. St. Laurent sat down and listened to my issues. He did not give me the impression he had any other patients- I was the number one and only focus during my visit. He explained my issues as well as did a really good drawing to make sure I understood. Highly impressed.
View on GoogleVery professional The entire staff and doctors were the best in every aspect. Friendly and explain things in a way you can understand. You leave with a feel good feeling about yourself.
View on GoogleYour Surgery Options
Gastric Bypass Surgery
Gastric bypass surgery involves dividing the stomach into two sections: a smaller upper section and a larger lower section. The small intestine is then connected to the upper portion of the stomach. After gastric bypass surgery, food will bypass the lower part of the stomach, allowing patients to feel full after consuming much less food. Although gastric bypass requires significant modifications to the stomach, it can help patients achieve a substantial amount of weight loss. Our surgeon will carefully assess your individual case to determine if gastric bypass or another type of bariatric surgery is right for you.
Gastric Sleeve Surgery
During gastric sleeve surgery, also known as sleeve gastrectomy, your bariatric surgeon removes a significant portion of stomach tissue, leaving a small section that resembles a thin, vertical “sleeve," which is then stapled shut. Having a smaller stomach limits the amount of food a patient can consume during a single meal. Over time, patients experience weight loss as their caloric intake becomes reduced. During a consultation, our surgeon can explain the full benefits of sleeve gastrectomy and discuss your needs and goals to determine if this bariatric treatment is right for you.
Loop Duodenal Switch
To perform a procedure known as duodenal switch, Dr. St. Laurent removes a large portion of the stomach and shortens the small intestine. Then, he will attach the intestine to the new, smaller stomach pouch. In order to reduce post-operative nutritional deficiencies, Dr. St. Laurent performs the SIPS (stomach intestinal pylorus-sparing surgery) technique. After a duodenal switch procedure, consumed food will bypass the upper portion of the small intestine, decreasing the amount of calories absorbed. This procedure can be revised or used to revise a previous type of surgery.
LAP-BAND
With the LAP-BAND system, Dr. St. Laurent places a LAP-BAND adjustable gastric band around the stomach, creating a smaller area for food. This decrease in size allows patients to feel as though they are full after eating only a small amount of food. After surgery, your caloric intake should drastically decrease, helping you to gradually lose weight. The LAP-BAND system offers several unique benefits. Most notably, it does not require significant modifications to your stomach or intestines. In addition, it can be easily reversed, should you decide in the future that the LAP-BAND system is not right for your lifestyle.
Revision Bariatric Surgery
In some cases, a patient at our Houston-area office will regain a significant amount of weight or experience complications following a bariatric procedure, necessitating a second surgery. Revision bariatric surgery may involve addressing an issue that arose from the initial procedure, or Dr. St. Laurent may convert one type of procedure into another. For example, we can use revision surgery to convert a gastric sleeve into a gastric bypass or duodenal switch, or convert LAP-BAND into a gastric bypass. Dr. St. Laurent will review your unique situation to determine the types of revision surgery that are right for you.

Take the First Step
Contact Us Today
At Northwest Endosurgical serving Houston, TX, we understand that choosing weight loss surgery is a major and potentially intimidating decision. If you are just beginning to research the possibilities of bariatric surgery, we applaud you for taking your health seriously and seeking a solution to obesity. Now, you can get one step closer to life-changing weight loss by scheduling a consultation with Dr. St. Laurent.
Consultations at our practice are informative, honest, and low-stress. Dr. St. Laurent won't shame you for your weight or try to sell you a surgical procedure that you don't need. Instead, he'll take time to get to know you and help you understand the benefits and risks of bariatric surgery.
You can request your consultation right now by filling out our online form or giving our Houston-area office a call.
Call Us: (281) 921-1890
Houston Recommends Dr. St. Laurent
Dr. St Laurent is one of those very special drs. You rarely find. He has spent so much time with me explaining things to me and and taking my calls all hours of nights and weekends. Yes weekends! While I felt bad about contacting him on a Sunday, he was right there to direct to the Er to help me get my issues under control. A truly kind and attentive dr. I only wish he could be my PCP. His office personnel is justas caring with Danielle and Michelle both taking their time to help me with anything. Poor Danielle fought my insurance company to get a procedure approved for a year. She finally got. It. Thank you all very much!
View on GoogleThe team at Northwest Endosurgical is amazing. A summarization of their practice could be, "We Care, and We'll Help You Get There". They are very good at what they do. Dr. St. Laurent made me very confident and comfortable during and after the procedure. The dieticians are excellent. They are very patient and supportive. The team stands out by providing accountability and care, without shaming. The entire staff works in sync with you and the rest of the team. What else is there to write; they may have helped save my life.
View on GoogleMeet Dr. St. Laurent
The Cost
of Bariatric Surgery
The price of bariatric surgery by Dr. St. Laurent varies on a case-by-case basis. In some cases, insurance may contribute to the cost of your procedure. However, there are many patients who could benefit from bariatric surgery, but do not meet the requirements for insurance coverage. Our practice serving Greater Houston offers several low-interest financing options that can help you budget for bariatric surgery; we also offer self-pay plans involving affordable monthly payments:
- Gastric Balloon Surgery: Starting at $215 per month
- Sleeve Gastrectomy: Starting at $335 per month
- Roux-en-Y: Starting at $683 per month
- Duodenal Switch Surgery: Starting at $736 per month
- Bariatric Revision Surgery: Starting at $736 per month
Bariatric Surgery Resources
Bariatric Surgery Candidacy
Bariatric surgery is not recommended for all patients who are overweight. Instead, these procedures are designed for patients who have a body mass index (BMI) above 40, a BMI of 35 and an obesity-related condition, or those who are more than 100 pounds above their ideal body weight. Dr. St. Laurent will evaluate your candidacy for bariatric surgery during a personal consultation. In addition to meeting physical criteria, candidates must be ready to make significant lifestyle changes to help maintain a healthy weight and avoid future complications.
Bariatric Procedure Guide
Before surgery, we provide patients with a bariatric surgery guide to help ensure a safe and successful procedure. Since proper planning is vital to the ultimate success of your weight loss surgery, the guide will include instructions for both before and after your treatment. You can refer to the guide for pre- and post-operative meal plans, as well as recovery and eating guidelines for the coming years. It is imperative that patients follow all behavior modification instructions and exercise recommendations after surgery for continued success.
Compare Surgery Options
We offer several weight loss surgeries, and each has its own set of benefits and important considerations. In order to help our patients make fully informed decisions about their care, we educate them about the differences between bariatric treatments. Each procedure involves a unique surgical technique and affects the body in different ways. In addition, the necessary lifestyle adjustments following surgery will be different depending on the procedure. During your consultation, Dr. St. Laurent will help you better understand the benefits and potential complications of each procedure.
Budgeting for Bariatric Surgery
Questions about the cost of bariatric surgery are usually at the forefront of our patients' minds. At our Houston-area practice, we do everything we can to help you afford weight loss surgery. We accept several forms of financing, offer monthly payment plans, and will help you maximize any available insurance benefits. We are upfront and honest about the cost of our weight loss services, so you won't have to worry about receiving a surprise bill. All questions about price and financing can be answered at your initial consultation.
Calculate Your Body Mass Index
Don't Tackle Weight Loss Alone
Request a Consultation
Weight loss journeys can feel isolating. When fighting obesity is a collaborative and supportive process, the journey becomes much easier. While only you can make the change for a healthier lifestyle, Dr. St. Laurent and his staff can support you at every step. From preparing for your visit to our Houston-area office to the end of the surgical process, we will be right at your side.
Contact our office serving Greater Houston to request a consultation with our surgeon.
(281) 921-1890
Why Patients Trust Us
Very friendly environment. Dr. spends time with you discussing your situation. All of the staff are very patient focused. They really exemplify listening to the patient, and taking time to explain.
View on GoogleI found Dr. St. Laurent and his team to be thorough, knowledgeable and professional regarding the entire weight loss, surgical journey. The care after surgery is comprehensive and lasts for a year. There are 2 dietitians on staff the offer unique, fact-based advice. I found that to be the differentiating factor in my decision to trust my medical care with NW Endo. I highly recommend, and have already referred my wife and close friend.
View on GoogleDoctors Trust Us With Their Care Dr. Alain Elbaz's Story
Nonsurgical Options Bariatric and Cosmetic Procedures
Gastric Balloon
You may not be ready to commit to the permanent effects of a surgical weight loss procedure like gastric bypass or sleeve gastrectomy. In that case, you can consider the gastric balloon. During a gastric balloon procedure, Dr. St. Laurent inserts a deflated balloon through your esophagus and into your stomach. Then, he inflates the balloon so it takes up a significant amount of space in your stomach. The treatment is safe, involves no incisions, and leads to healthy weight loss.
Body Contouring
Our practice serving Greater Houston offers plastic surgery after substantial weight loss and uses the InMode body contouring system to help patients tone their muscles, tighten excess skin, and eliminate stubborn fat deposits.
Laser Treatments
We use the Icon™ laser to target fine lines, spider veins on the face, and stretch marks on the body. We also use RF technology to eliminate stubborn fat deposits.
"They treat you like so much more than a patient."
Dr. Laurent seemed genuinely interested in my health and spent a significant amount of time to explain my diagnosis thoroughly, along with providing several remediating options with varying associated costs and benefits (pros/cons). His recommended solutions were focused on mitigating my condition, rather than just treating my symptoms, unlike most GI doctors tend to do. I was very impressed by his wealth of knowledge and the fact that I never felt rushed during my Q&A. In addition, my appointment was on-time and the front office staff were very professional and amiable. I totally recommend Dr. St. Laurent for the most comprehensive, efficient, and positive patient experience!
View on GoogleDr. St. Laurent and his staff go above and beyond ANY physician I have ever been to. I have had 2 in office visits and each time Dr. St. Laurent has been patient, thoroughly goes in detail his recommendations and you don't feel rushed. I have only had the pleasure of dealing a few of the staff and they all are very personable and treat you like so much more than just a patient. I highly recommend Dr. St. Laurent to ANYONE.
View on GoogleFrequently Asked Questions About Bariatric Surgery
How do I get insurance to cover bariatric surgery?
Plans differ, but in general, the ones that contribute to the cost of bariatric surgery have requirements such as having a BMI of 40 or higher (or 35 with a comorbidity such as type-2 diabetes), a documented history of weight loss efforts, and stopping smoking. Our Houston-area bariatric practice is glad to work directly with your insurance provider to determine if you qualify, or to help provide the required documentation.
How much does bariatric surgery cost?
Our practice prices roux-en-y and other bariatric surgery procedures on a case-by-case basis. Depending on your BMI and other data, you may qualify for insurance coverage. We also offer a variety of financing options, as well as self-pay payment plans that allow you to pay in monthly installments.
Is bariatric surgery safe?
All surgical procedures carry some degree of risk, including bariatric surgery. Risks associated with surgical weight loss include dumping syndrome, kidney stones, and failing to lose the desired amount of weight. The surest way to minimize the risks of bariatric surgery and experience the very best benefits is to choose a reputable surgeon.
Which vitamins will I need to take after bariatric surgery?
Each bariatric surgery requires a different vitamin regimen afterward. For example, gastric bypass and gastric sleeve patients usually take a complete multivitamin, B12, calcium with Vitamin D, iron and Vitamin C, and Vitamin D. Dr. St. Laurent is a bariatric surgeon who will provide you with the education, counseling, and nutritional guidance you need to begin and maintain a new chapter of health in your life following bariatric surgery.
Patients Share Why They Chose Our Practice
Dr. St. Laurent and his entire staff is great. They care about their patients. They listen and are very responsive to requests and questions. Highly recommend!
View on GoogleI don't even know where to start, other than straight to the point, Dr. St Laurent is amazing, wonderful, world's best bed side manners, takes your health serious and extremely honest on what is possible and what is not.
View On Google